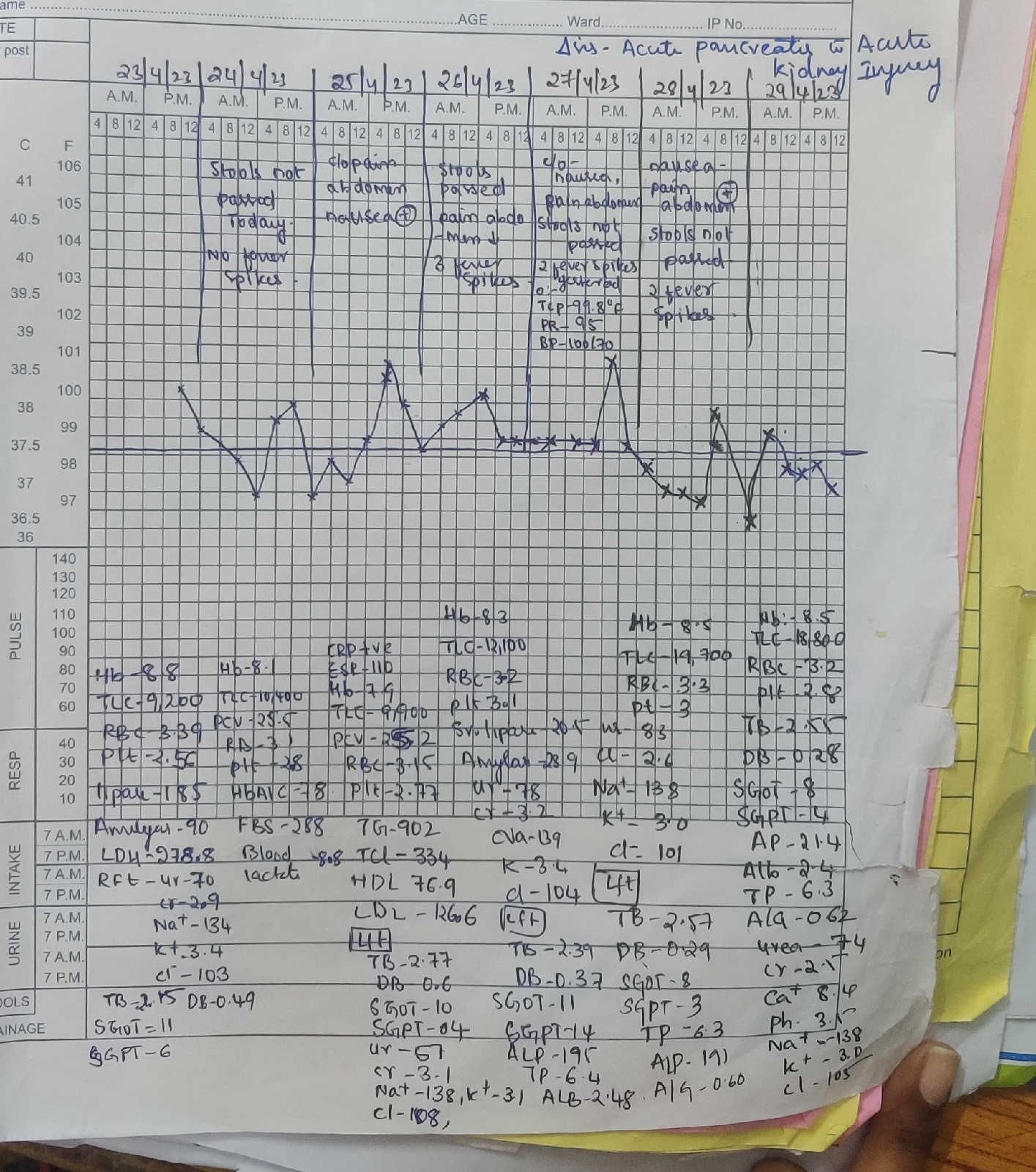
40yr/F with acute pancreatitis
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
acute history of pain abdomen & vomiting’s since 4 days
HOPI
Patient was apparently asymptomatic 4days back now presenting with complaints of pain abdomen originated at left hypochondrium and lumbar region (VAS 7 score) then became diffuse in type over 10 to 12 hours (VAS 10)
Worst pain she ever had), squeezing type of pain with occasional coliky type, associated with vomiting’s 2-3 episodes non bilious , non-projectile, non-blood tinged with food particles as content. Passing stools small amount (as fecal pellets of goat - described by patient) didn’t pass flatus since 2 days.
history of bloating, belching since 5 years using antacids.
H/o Passage of hard stools since 2 months
Past history
K/c/o diabetes since 7yrs
Not a known case of htn, thyroid,tb, epilepsy.
Treatment history:
weekly she used to take 2-3 sachets of ENO (antacids)
Personal history:
Diet:mixed
Appetite -reduced
Bowel-constipation since 5months
Bladder -regular
No addiction
MARRIAGE & OBSTETRIC HISTORY:
Married at the age of 17 years , non-consanguineous.
FIRST child at 18 years - death of the first child at 24years due to varicella zoster.
2nd child at age of 21 years - gave birth to female child , now married
3rd child at the age of 23 years -gave birth to female child , now married
4th child at the age of 24years - gave birth to male child currently 10th class.
LMP-23/04/23
FAMILY HISTORY:
Mother is hypertensive and expired due to cerebrovascular accident and post stroke complications after 6 months.
General examination
Patient is conscious, coherent Cooperative
Pallor present
bilateral pitting type of pedal Edema present with scratch marks on both lower limbs (pruritus due to possible diabetic dermopathy)
No icterus, cyanosis, clubbing, lymphadenopathy.
She used to colour her hair since 8 years (early whitening of hairs at 28 years – probable zinc and other nutritional deficiencies)
Looks grossly dehydrated with sunken eyes, dry oral mucosa and tongue with delayed capillary refill time (more than 3 seconds)
SYSTEMIC EXAMINATION:
EXAMINATION OF THE ORAL CAVITY
NO Oral thrush, NO tonsilar enlargement & pharyngeal deposits, NO post nasal drip, NO fetor hepaticus, Fair oral hygiene, no dental caries and no gum hypertrophy.
ABDOMEN
INSPECTION:
1. Shape – distended-uniform
2. Flanks – full
3. Umbilicus – central, Shape-slit like and nodules.
4. Skin – stretched, no scars & sinuses, striae present, scratch marks.
5. No Dilated veins – front/back
7. Movements of the abdominal wall,NO visible gastric & intestinal peristalsis.
8. Hernial Orifices - normal
9. NO Renal angle tenderness
PALPATION
Superficial Palpation – Tenderness present at left hypochondrium and lumbar region, no local rise in temperature.
Deep Palpation
1. Liver: inferior edge palpable, smooth non nodular.
2. Spleen non palpable and non-tender when palpated in the Left Hypochondrium.
3. Kidney non-tender and non palpable in the Right/Left Lumbar.
4. Abdominal Girth - 79cms
5. Distance between the Xiphisternum-Umbilicus and Umbilicus-Pubic Symphysis equal 17 cms.
6. No Murphy’s Punch/Renal angle tenderness.
PERCUSSION:
1. Puddle’s sign present suggestive of mild fluid collection in abdomen.
2. Percussion of Liver for Liver Span - 13cms
AUSCULTATION:
1. Bowel sounds – sluggish
2. No Bruit – Aortic, Hepatic, Renal Bruit
3. No Venous Hum.
CARDIOVASCULAR SYSTEM:
No raised Jugular venous pressure
Apex beat in 5th Intercostal space on left mid clavicular line
S1 and s2 heard. NO murmurs.
EXAMINATION OF RESPIRATORY SYSTEM:
No tracheal deviation
Respiratory movements are bilateral symmetrical
Resonant percussion in all lung field’s
Normal vesicular breath sounds.
EXAMINATION OF NERVOUS SYSTEM:
Higher mental functions intact
All Cranial nerves on both sides are intact
No motor deficits
Sensory system :
Fine touch - absent below both ankles
Vibration - delayed in both lower limbs ( 6sec at ankle, 8 sec at knee ) and upper limbs ( 9sec in upper limb )
Gait normal
Gastroenterologist consultation was taken :
Advised for IgG4 antibodies , ANA and MRCP.
Provisional diagnosis
Acute pancreatitis secondary to triglycerides with acute kidney injury , hypokalaemia
Diabetic nephropathy
Treatment:
NBM till further adress
Iv fluids 10ns@100ml/hr
Inj.pan 40mg /iv/od
Inj.zofer 4mg /iv/sos
Inj.optineuron 1amp in 500mlns/iv/od
Inj.neomol 1gm/iv/sos
Inj .metrogyl 500mg /iv/tid
Inj.ciproflox 200mg /iv/bd
Tab.sporalac 2tabs /po/tid
Monitor vital hrly
Inj.tramadol 1amp on 100ml ns /iv/sos
Strict i/o charting
Discharge summary
she was referred to higher centre as she is clinically deterioration of symptoms and need for MRCP and patient and patient atternder explained about the need of MRCP
In our hospitals we done all the requried investigation and given symptomatic treatment
.




Comments
Post a Comment