This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input..
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan .
This is a case of 35yr old presented to casuality with the complaints of yellowish discolouration of eyes since 1 week,
Dark coloured urine since 1 week.
HOPI:
He was apparently asymptomatic 1 week back then he developed yellowish discolouration of eyes since 1 week which was insidious in onset,gradually progressive
Dark coloured urine since 1 week which is on and off .patient complaints of pale coloured stools since 1 week,not blood stained.
Patient complaints of swelling of both lower limbs,since 1 week extending upto the ankle,pitting type,aggrevated on walking and relieved by rest.
No complaints of pain abdomen,abdominal distension/bloating.
No complaints of nausea,vomiting,chestpain,shortness of breath.
Past History:
Not a known case of Dibetes,Hypertension,Tuberculosis,Asthma,Cva ,Cad,Thyroid disorders.
Family History:
Not relevant .
Personal History:
Diet: mixed
Appettite:normal
Bowel and bladder: Regular
Sleep: Adequate
-He is regular alcoholic since 10 yrs drinks 150ml per day
-Doesnot smoke
GENERAL EXAMINATION
Patient was conscious,coherent cooperative
Moderately build and moderately nourished
well oriented to time ,place and person
cyanosis: absent
Lymphadenopathy: absent
Edema : absent
VITALS:
Temp: febrile
BP: 100/60 mmHg supine position
PR- 98 bpm
RR- 16 cpm
SYSTEM EXAMINATION:
Abdominal examination-
INSPECTION
On Inspection Abdomen is scaphoid,
no abdominal distension,
umbilicus is central and inverted ,
no scars ,sinuses
PALPATION
All inspectory findings are confirmed
PERCUSSION : No significant findings
AUSCULTATION: bowel sounds heard
RESPIRATORY EXAMINATION
trachea central,
normal respiratory movements,
normal vesicular breath sounds.
CARDIOVASCULAR SYSTEM
S1 ,S2 heard ,no murmurs
CNS EXAMINATION
CNS examination
CNS examination
HIGHER MENTAL FUNCTIONS:
Conscious, coherent, cooperative
Appearence and behaviour:
Emotionally stable
Recent,immediate, remote memory intact
Speech: comprehension normal, fluency normal
CRANIAL NERVE:
All cranial nerves functions intact
SENSORY FUNCTIONS
SPINOTHALAMIC TRACT
Pain , temperature ,presure- intact in all limbs
Posterior column:
Fine touch, vibration and proprioception are intact
MOTOR SYSTEM :
Right Left
Bulk:
Inspection. N. N
Palpation. N. N
Tone:
UL. N. N
LL. N. N
REFLEXES
B T S K A P
R 2+ - - - - Flexor
L 2+ - - - - Flexor
CEREBELLUM:
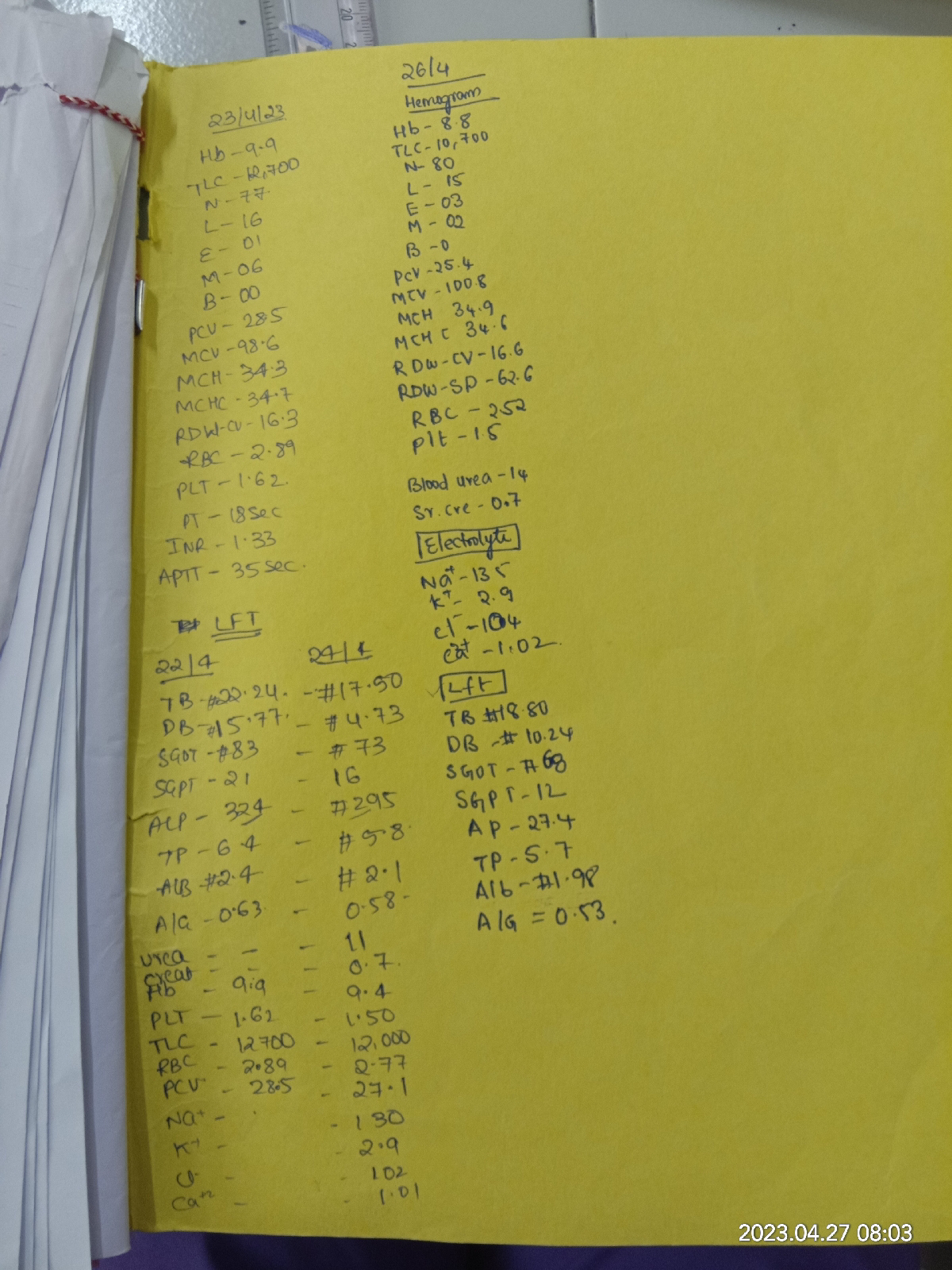
Investigations:
chest x ray
ECG
ABG
Provisional diagnosis:
Alcoholic Hepatitis
Treatment:
INJ.TREMADOL 1amp 100mlNS IV /SOS
INJ .UDILIV 300mg PO/BD
TAB.RIFACXMIN 550MG PO/BD
TAB.MUCINOC PO/BD
INJ.KCL 2AMP IN 500ML NS IV OVER 6 HRS
SYP.HEPAMERZ 15ml/PO/BD
SYP LACTULOSE PO/OD
TAB.PANTOP 40MG PO/OD
TAB.ULTRACET 1/2 tab. PO/BD
BP MONOTORING HOURLY
INJ.THIAMINE 1 amp in 100ml NS/IV/BD












Comments
Post a Comment