65yr old male with SOB since 2days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment
A 65 year old male came to OP with chief complaints of fever since 1 week and SOB since 2 days.
Patient was apparently asymptomatic 4 months back after which he developed pedal edema which was on and off,pitting type.
He developed SOB grade 2 which is aggravated on activity and decreased on taking rest. No History of orthopnea,PND.
No history of chest pain, palpitations,dry cough and facial puffiness.
History of fever since one week which is high grade, continuous.
Patient has history of wound with bleb over the right leg second toe after which he developed fever.
He has persistent rise in creatinine value since past 4 years
Past history:-
Known case of renal failure since 5 months
Known case DM 2 since 10 years and is on medication.
Known case of HTN since 15 years and is on medication.
Personal history:-
Diet-mixed
Appetite -adequate
Bowel and bladder movements:-decreasesd urinary output,bowel movements regular
Sleep - adequate
Addictions - none
Family History:
Not significant
General examination:-
Patient is conscious, coherent, cooperative
Moderately built, moderately nourished
Pallor present,
Icterus-absent
cyanosis-absent
clubbing-absent
Koilonychia-Absent
Lymphadenopathy -absent
Pedal edema-absent

Vitals -
BP-120/80mmhg
PR-100bpm
RR-22cpm
Spo2-99
Temp- afebrile
Grbs - 271mg/dl
Systemic examination -
Abdominal examination-
flat,all quadrants are moving according to respiration .umbilicus is central and inverted,no engorged veins,no scars,no sinuses
Tenderness present in right hypochondrium and epigastric region .
No guarding
,no rigidity,liver dullness in 5th intercoastal space, bowel sounds present.
Respiratory system-inspection- trachea central,normal respiratory movements,normal vesicular breath sounds.
Cardio vascular system- S1 ,S2 heard ,no murmurs
CNS Examination: patient is not conscious,
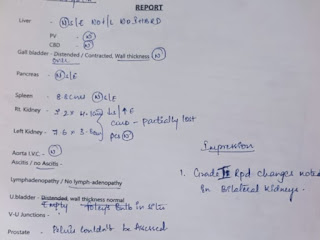
Investigation -
Provisional diagnosis -
Altered sensorium secondary to ?uremic encephalopathy,Urosepsis,left lower leg diabetic foot/ulcer
Uncontrolled sugars
K/c/o DM since 10yrs
K/c/o HTN since 15yrs
Treatment:
1.Ivf- ns@50mlhour
2.inj. piptaz 4.5 gm iv stat ( day 1)
3.inj lasix 40mg/iv/bd if sbp > 110
4.inj neomol 1gm if temp >101 ° f
5. Inj HAI sc/ tid
6. tab nodosis 500mg/rt/bd
7. tab orofer rt/of
8.rt feeds 100ml water every 2nd hourly,200ml milk every 4th hourly
9.grbs every 2nd hourly and inform pg
10.monitor vitals hourly
11.strict iv charting







Comments
Post a Comment